EndTidalCO2
Last updated: 6 Aug 2024 | 104437 Views |

Capnograph press to Download PDF
Carbon dioxide
Carbon dioxide in the human body is produced by human cellular respiration. and then circulates with blood to the lungs through red blood cells and plasma exchange with oxygen at the alveoli of the lungs and exhale through the exhalation as shown in Figure 1.
Figure 1 shows the excretion of carbon dioxide into the alveoli.
We can measure the amount of carbon dioxide. both in the breath and in the blood The value measured by the breath represents If the body works normally, the circulatory system works normally. normal heart beat It will be able to measure the carbon dioxide in the breath normally. On the other hand, if the heart does not work well or does not beat, gas exchange will not occur. This causes the carbon dioxide in the breath to decrease.

Capnography
It is a measure of carbon dioxide in the breath. It is measured by lung function only. It is usually measured through an endotracheal tube.
The method for measuring carbon dioxide using chemical principles is calorimetric device, which uses filter paper that can change color according to different CO2 values, but cannot tell the value in numbers or graphs.
At present, we use the principle of conduction of light infra-rate spectrometry divided into two types:
1. Main stream is the measurement when the gas passes immediately, it is real time and no loss of air in the respiratory tract.
2. Side stream is air intake. Analyze it in the device and measure it. It takes more than 2-3 seconds, but other gases can also be analyzed
The values that can be measured are as follows:
1. End-tidal carbon dioxide (PETCO2) is the concentration of carbon dioxide in the exhaled breath at max. In humans, it is usually PETCO2 35-40 mmHg.
2. Capnography is a curve showing the concentration of carbon dioxide at different times.
reading method Capnograph และ Capnogram
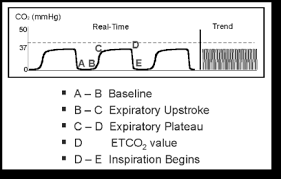
⁃ Respiratory baseline (A-B) represents free CO2 from dead space without gas exchange. The value should be zero.
⁃ Expiratory Upstroke (B-C) represents exhale CO2 from dead space and alveolar gas from some acini with little transit time.
⁃ Expiratory Plateau (C-D) mainly represents exhale CO2 from the alveolar.
⁃ End-tidal CO2 (D) represents the maximum exhaled CO2 value.
⁃ Inspiratory Downstroke (D-E) represents breathing free CO2.
⁃ Trend: Slower capnography tracing will narrow the waveforms so that the trend of plateau value can be seen.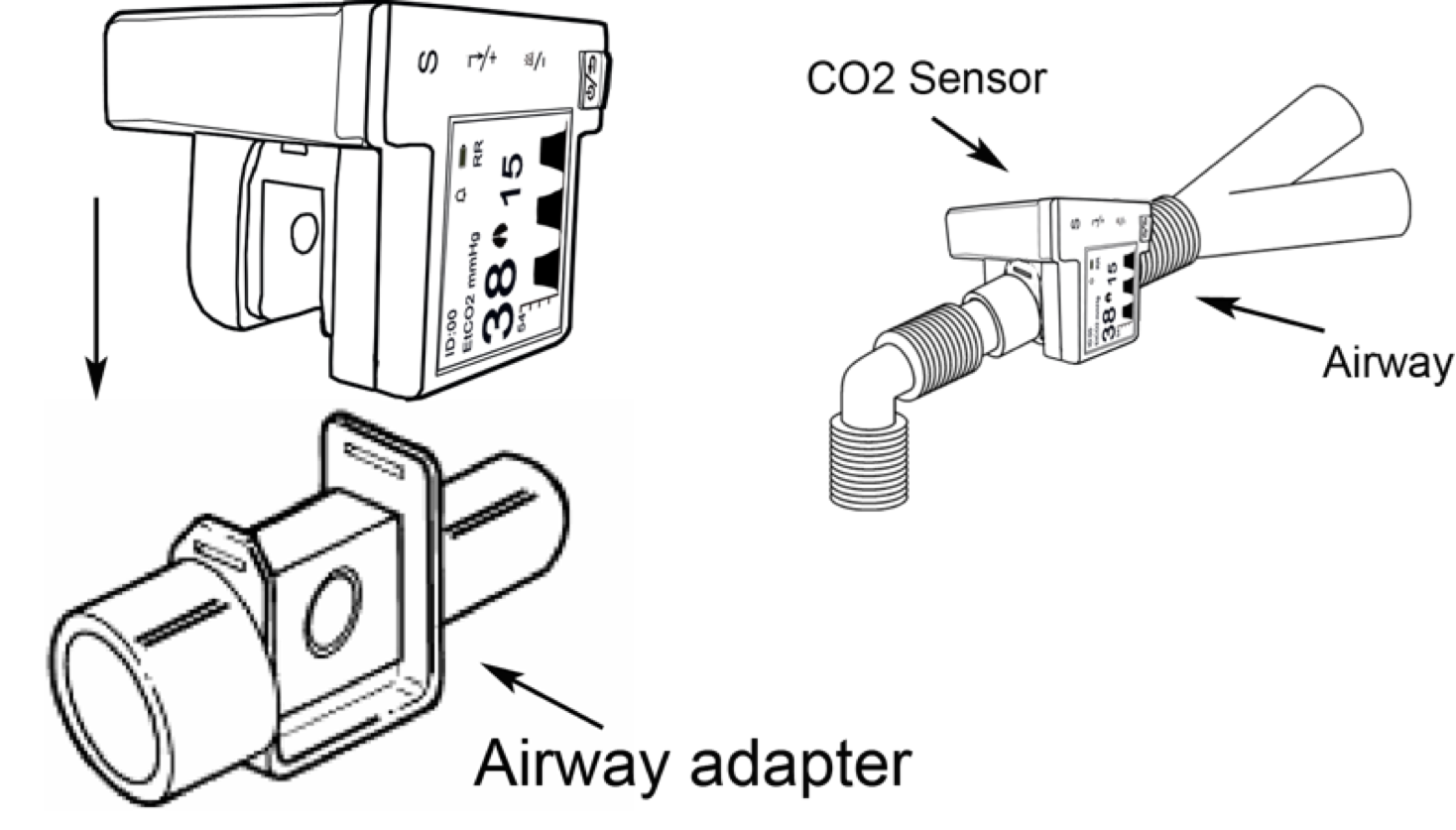
benefit Capnography
During chest compressions, patients in cardiac arrest, exhaled carbon dioxide can also show good cardiac output, with end-tidal CO2 (PETCO2) greater than or equal to 10 mmHg indicating good compression performance. causing gas exchange in the lungs If during chest compressions the cardiac pump has a PETCO2 value greater than 40 mmHg, it may show ROSC (Return Of Spontaneous Circulation).
Capnography is also used to determine the insertion of a tracheal tube into the windpipe. If there is a consistent increase in endotracheal carbon dioxide, it indicates that the tracheal tube is in the trachea, the sensitivity and specificity are more than 95%, but sometimes there may be residual carbon dioxide in the stomach. When intubation into the esophagus, PETCO2 readings are readable, but they gradually decrease with each assisted breathing until they disappear.
We take advantage of safety during patient transport by monitoring End-tidal CO2 (PETCO2) values because while moving patients do it with difficulty and changes in the patient's status all the time When the patient's symptoms worsen Both the circulatory system and the respiratory system can be alerted quickly, especially the respiratory system and the tracheal tube, such as a broken endotracheal tube.
Cardiopulmonary Resuscitation (CPR) varies with coronary perfusion pressure during CPR. End-tidal CO2 values can tell coronary perfusion pressure when correcting all reversible causes. Then continuous chest compressions for 20 minutes and then End-tidal CO2 measured less than 10 mmHg for 20 minutes was the decision criterion. stop saving lives (Resuscitation)
Related content
ManualJiaCO2
1 May 2017
ACLS Recorder Form
1 Sep 2020
ACLS Drug
5 May 2017
First Aid For the general public
30 Jul 2024







